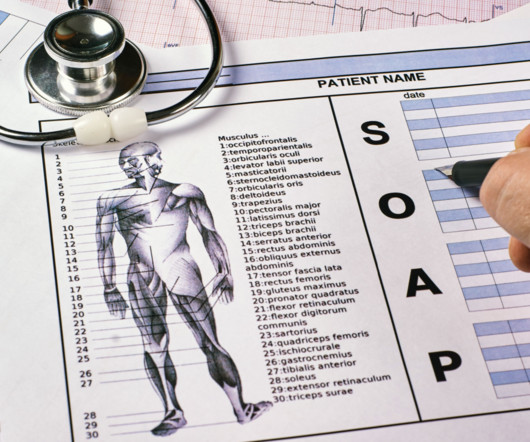
Basics of Medical Documentation: What Aspiring Medical Billers and Coders Need to Know
Northwest Career College
JULY 3, 2025
Accurate documentation is essential for medical billing and coding, but many beginners struggle to understand the technical terms and guidelines. Without accurate medical documentation, insurance claims can be delayed or denied, frustrating patients and physicians. What is Medical Documentation?






































Let's personalize your content